Oct . 02, 2025 16:50 Back to list
Plasmodium Detection via PCR: Faster, Accurate—Why Us?
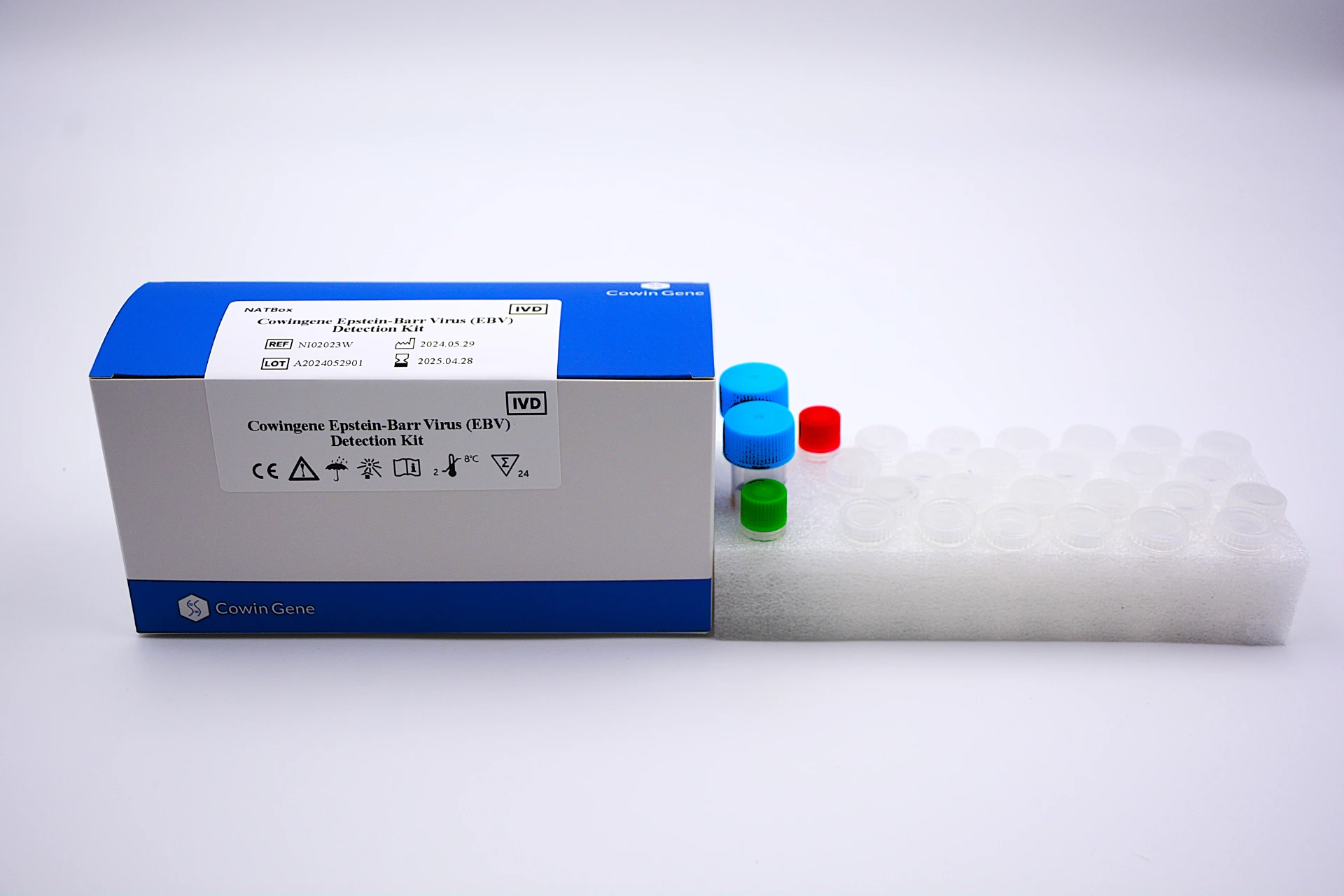
Cowingene Plasmodium Detection Kit: Field Notes, Lab Specs, and What’s Changing in Malaria Dx
If you’ve been following malaria diagnostics the past couple of years, you know the market is shifting fast—from purely lateral-flow quick checks to molecular confirmation in compact workflows. When people ask me what’s practical today, I point them to plasmodium detection that’s designed for routine lab use but doesn’t feel like a moonshot project. To be honest, I like kits that balance speed with traceability, and Cowingene’s offering hits that note surprisingly well.
Trends? Three big ones: confirmation of low parasitemia (think travelers or post-treatment monitoring), interoperability with existing lab gear, and stricter QA. Many customers say they don’t want a black-box. They want a kit that plays nicely with their SOPs, barcode systems, and—ideally—ISO/CLSI expectations. That’s where genus-level plasmodium detection kits, paired with clear IFUs, have been landing lately.
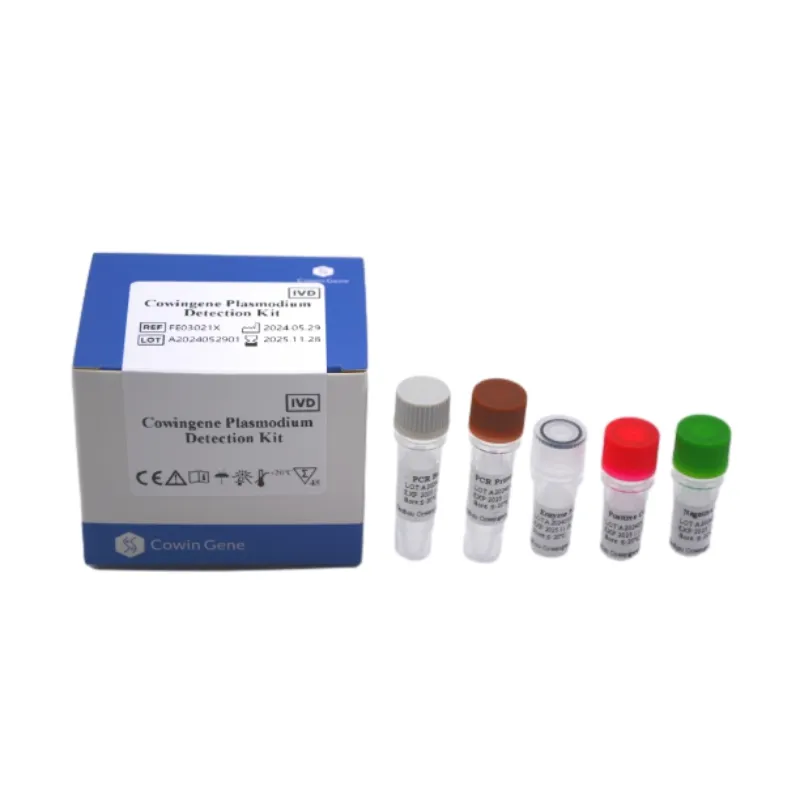
Product snapshot and specs
Origin: NO.28, Xinlin Road, Taizhou city, Jiangsu Province, China. It’s a molecular assay kit focused on genus-level plasmodium detection for whole blood, meant to fit into standard lab workflows.
| Product Name | Cowingene Plasmodium Detection Kit |
| Validated Specimen | Whole blood (EDTA or ACD) |
| Analyte | Plasmodium (genus); 1 tube/test |
| Intended Use | Qualitative plasmodium detection from anticoagulated blood |
| Storage / Service Life | 2–8°C; shelf life ≈ 12–24 months (real-world use may vary; see IFU) |
| Compliance Signals | Designed for labs operating under ISO 15189; vendor typically supports ISO 13485 QMS documentation |
Process flow (materials, methods, standards)
- Materials: EDTA/ACD blood, kit reagents, controls, calibrated pipettes, PPE, and a compatible thermal platform (per IFU).
- Method overview: Nucleic-acid–based amplification with internal control; genus-level plasmodium detection.
- Suggested testing standards: CLSI EP05 (precision), EP17 (LoD), EP07 (interference). Stability studies aligned with EN ISO 23640 are typical.
- QC: Run positive/negative controls each batch; document traceability against lab LIMS.
Indicative performance (internal validations reported by comparable kits): LoD ≈ 1–5 parasites/μL; Positive agreement ≈ 97–99%; Negative agreement ≈ 98–100% against composite reference (microscopy + PCR). Always verify locally—matrix effects are real.
Where it’s used
Hospital labs, border/travel clinics, NGO field programs (with bench-top thermals), pharma surveillance cohorts. A lab in Southeast Asia told me they use it to confirm low-density infections post-RDT; another in West Africa uses it for mixed-infection screening during rainy season. It seems that predictable turnaround and clear QC flags mattered more than flashy UI.

Why labs pick it (and when they don’t)
- Advantages: Genus coverage, low parasitemia detection, compatible with routine sample tubes, straightforward QC.
- Limitations: Requires basic molecular setup; not a field-only strip. For purely remote triage, RDTs still win.
Vendor comparison (quick take)
| Vendor | Assay type | Turnaround | LoD (≈ parasites/μL) | Notes |
|---|---|---|---|---|
| Cowingene Kit | Molecular (genus) | ~1–2 hrs | ≈1–5 | Good for low-density confirmation |
| Popular RDT (HRP2/pLDH) | Lateral-flow | 15–20 min | ≈100–200 | Great triage; HRP2 deletions a caveat |
| Generic qPCR platform | Open PCR | 1.5–3 hrs | ≈0.5–2 | Ultra-sensitive; higher setup needs |
Customization and rollout
OEM/private label, bilingual IFUs, lot-specific COAs, and kit sizes for 24/48/96 tests are common asks. I guess the best advice: lock down your validation plan (CLSI-style) before bulk ordering.
Mini case notes
- Provincial hospital: Reported ≈30% reduction in microscopy confirmations after adopting molecular plasmodium detection for low-density samples.
- Mining camp clinic: Switched to genus-first molecular screen, then species typing at reference lab; fewer missed mixed infections, according to their QA lead.
Citations
- WHO. Malaria diagnostics and treatment guidelines. https://www.who.int/teams/global-malaria-programme
- CDC. Malaria Microscopy & Laboratory Guidance. https://www.cdc.gov/malaria/diagnosis_treatment
- CLSI EP17-A2. Evaluation of Detection Capability for Clinical Laboratory Measurement Procedures.
- CLSI EP05-A3. Evaluation of Precision of Quantitative Measurement Procedures.
- EN ISO 23640. In vitro diagnostic medical devices — Evaluation of stability of IVD reagents.
Related PRODUCTS
-
Understanding Monkeypox Testing PCR – Global Health & Diagnostic Insights
NewsNov.24,2025 -
Comprehensive Guide to Monkey Pox Detection: Methods, Applications & Innovations
NewsNov.23,2025 -
Essential Guide to Monkeypox Detection: Technologies, Applications & Future Trends
NewsNov.23,2025 -
Understanding Strep B Test Cost: Global Insights and Healthcare Impact
NewsNov.22,2025 -
Group B Strep DNA Test – Fast, Accurate Screening to Prevent Neonatal Infection
NewsNov.21,2025 -
Essential Guide to Group B Strep Test Kits: Benefits, Uses & Innovations
NewsNov.20,2025